Hi All,
In this article, we will discuss how women’s and men’s bodies differ, why women are systematically excluded from research studies, and what this means for women’s health.
To note, the majority of references and data are from the book “Invisible Women” by Caroline C. Perez, which won the Science Book Prize and the FT & McKinsey Business Book of the Year Award. (As always, full list of sources at the end.)
The Drugs Don’t Work
How do women’s and men’s bodies differ, why are women systematically excluded from research studies, and what does this mean for women’s health?
How do women’s and men’s bodies differ?
Historically it has been assumed that the only fundamental differences between male and female bodies were the size and reproductive function. So, for years the medical field (research, education, and practice) has been focused on a male norm, with everything that falls outside being considered ‘atypical’ or ‘abnormal’.
Today, we know that there are sex differences in every tissue and organ system in the human body. Also, the prevalence, course, and severity of the majority of common human diseases differ in men and women.
We will get into more details below but let’s start with some examples:
- Men and women have a different metabolic system. Women tend to have a higher body fat percentage and a lower base metabolic rate. Also, blood flow is greatest to fat tissue in women, while blood flow is greatest to skeletal muscle in men. à Men and women metabolise medication differently yet drugs (including anaesthetics and chemotherapeutics) are given in gender-neutral dosages, which puts women at risk of overdose. Also, male gut transit times are around half the length of women’s, meaning women may need to wait longer after eating before taking medications that must be absorbed on an empty stomach. Also, kidney filtering is faster in men.
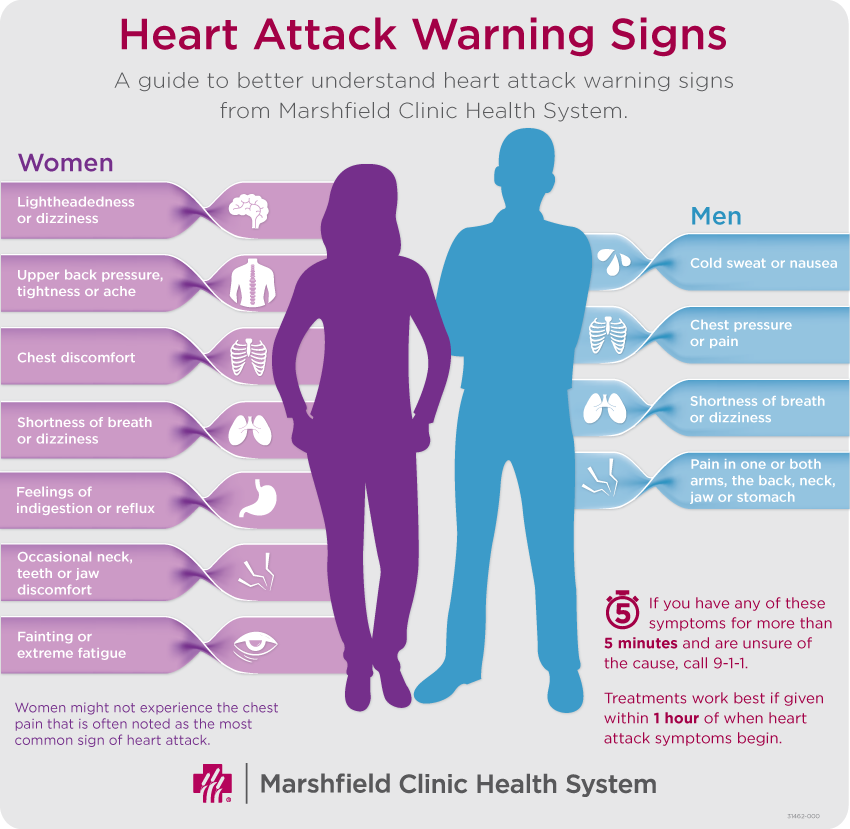
- There are sex differences in the fundamental mechanical workings of the heart. Only one in eight women who have a heart attack report the classic male symptoms of chest pain. (More details on the heart below.)
- There are sex-specific responses to vaccines. Women develop higher antibody responses and have more frequent and severe adverse reactions to vaccines. A 2014 paper proposed developing male and female versions of influenza vaccines.
- PH levels are significantly different in men and women. Women have lower (i.e., more acidic) skin and saliva pH levels which cause women e.g., more dental problems.
- There are sex differences in lung capacity even when these values are normalised to height. Also, women are 20-70% more likely to develop lung cancer.
- Autoimmune diseases affect 8% of the population of which 80% are women.
“For millennia, medicine has functioned on the assumption that male bodies can represent humanity as a whole. However, women are not just smaller men: male and female bodies differ down to a cellular level.”
So, if we know that these differences impact nearly everything (diet recommendations, sleep, medication, development/diagnostics/treatment of diseases, exercise, the cardiovascular system, (…)) then why are we still excluding women from the majority of clinical trials?
Why are women (and female animals) systematically excluded from research studies?
The most obvious and dominant reason is that women and men have different hormonal systems. While men’s hormones mainly run on a 24h cycle, women’s hormones run on a ~28day cycle and fluctuate daily (depending on the phase of the menstrual cycle). Also, hormones change peri/post-menopause. Researchers have argued that female bodies (both human and animal) are “too complex and too variable” to be tested on and that it makes research “too costly”.
Other researchers advocated against the inclusion of women because the new studies could not be compared to previous findings, as there were no women included in the past. This makes e.g., meta analysis of research papers harder. (Perez’s comment on/to this point: Talk about adding insult to injury.)
Overall, the integration of women is seen as “burdensome” and the exclusion is accepted on the basis of “simplification”.
This has led us to the following situation:
- Clinical trials are presented as valid for men and women even when women were excluded from the study – this is also the case in studies on topics where sex differences have long been established, e.g., depression. For example: Despite knowing that the metabolic system works differently in men and women, in 2017 a study was published and gained media attention as the researchers proposed “a possible treatment for metabolic diseases.” The study included no women at all. On top, researchers failed to acknowledge this as an issue and only criticised the relatively small sample size in the limitations section of their research paper.
- Even conditions that are known to cause the greatest morbidity and mortality in women failed to incorporate sex-specific information. (Meaning if women were included in the study, this is either not stated at all and/or the data is not analysed by sex.
- A wide range of medication that is specifically marketed towards women is not (or rarely) tested on women. For example:
- When the “female Viagra” was found to potentially interact negatively with alcohol, its manufacturer (Sprout Pharmaceuticals) decided to run a trial but recruited 23 men and 2 women despite the known fact that 1) alcohol absorption differs between men and women and 2) “female Viagra” is a product marketed specifically towards women. Also, they did not sex-disaggregate the data, so the results from the two women recruited are invisible.
- Valium was aggressively marketed towards women for decades (for conditions ranging from anxiety to epilepsy). However, a paper in 2003 pointed out that “mother’s little helper” was never tested in clinical trials with female subjects.
- Animal studies on female-prevalent disease did not include female animals. A 2014 paper found that of studies on female-prevalent diseases that specified sex (44%), only 12% studied female animals. Even when both sexes are included there is no guarantee the data will be sex-analysed: one paper reported that in studies where two sexes were included, two-thirds of the time the results were not analysed by sex.
- If women are included, researchers usually recruit women who are post-menopause or are tested in the early follicular phase of their cycle, when hormone levels are closest to the ‘male norm’. However, this does not represent real life where women go through all phases of the cycle and this impacts the effects drugs have on women. So far, menstrual-cycle impacts have been found for antipsychotics, antihistamines and antibiotic treatments as well as heart medication. Some antidepressants have been found to affect women differently at different times of their cycle, meaning that dosage may be too high at some points and too low at others. Perez: “Women are also more likely to experience drug-induced heart-rhythm abnormalities and the risk is highest during the first half of a woman’s cycle. This can, of course, be fatal.”
This brings us already to the next point:
What are the consequences of this for women’s health?
In short, many drugs on the market do not work on women or have adverse effects. Women are also more likely to be misdiagnosed and mistreated as the symptoms for many diseases differ; however, the symptoms in women are not known sufficiently. In addition, drugs that could work on women do not get developed as they are ruled out at the animal testing stage when the drug doesn’t work on male mice. Also, we know very little about women’s reproductive system and conditions affecting women exclusively.
Drugs & medical advice don’t work on women or have adverse effects:
For example:
- Some drugs used to break up blood clots immediately after a heart attack can cause significant bleeding problems in women. Other drugs that are commonly prescribed to treat high blood pressure have been found to lower men’s mortality from heart attack – but to increase cardiac-related deaths among women.
- In 2000 the FDA forced drug manufacturers to remove phenylpropanolamine (a component of many over-the-counter medications) from all products because of reported increased risks of bleeding into the brain in women, but not in men.
- A series of papers warned against resistance training if you have high blood pressure. While this is true for men, it has later been shown that it does lower blood pressure in women and that it also helps to counteract osteopenia and osteoporosis, both of which women are at high risk for post-menopause (a stage of life every living woman goes through).
- The recommendation for diabetics to do high-intensity interval training doesn’t help female diabetics. The reason for this is not known yet.
A 2015 research paper states:
“The specific effect on women of a huge number of existing medications is simply unknown.”
Women are misdiagnosed and mistreated:
This article mainly focuses on issues around medication but I want to flag that the problems around differing symptoms and resulting misdiagnoses are as relevant and important. Today, we will look at one example: the heart.
As mentioned above, women experience different symptoms during a heart attack, which has led to many delayed diagnoses (see graphic below). Also, women have different electrical heart signals which are associated with an increased risk of acute complications during primary pacemaker implantation (independent of age or type of device implanted). Here’s a powerful example: a CRT-D (device used to correct a delay in the heart’s electrical signals) is used if the heart takes 150 milliseconds or longer to complete a full electrical wave. However, this threshold is not applicable for women as it would need to be 20 milliseconds lower. This has led to women not getting treated (as their hearts didn’t meet the male standard) which resulted in avoidable heart failure for hundreds of women.
The CRT-D is by far not the only piece of medical tech that doesn’t work on women (if used based on instructions developed for male bodies). A 2014 analysis found that only 14% of post-approval medical-device studies included sex as a key outcome measure and only 4% included a subgroup analysis for female participants. In addition, in 2013, a supposedly revolutionary artificial heart was developed that was too big for women. Its designers were working on a smaller version that fits women but years after the default male one.
Medication which works on women does not get developed (if it doesn’t work on men):
What is the number of drug treatments that might be beneficial to women but never reach human testing because they are ruled at the cell and animal trial stage (tested on male bodies)?
Sex differences in animals have been consistently reported for nearly fifty years, and yet a 2007 paper found that 90% of pharmacological articles described male-only studies. In 2014 another paper found that 22% of animal studies did not specify sex, and of those that did, 80% included only males.
We don’t know how to treat pregnant women:
The WHO warns that many diseases can have particularly serious consequences for pregnant women, or can harm the foetus. However, because of their routine exclusion from clinical trials we lack solid data on how to treat pregnant women for pretty much anything. Perez: “We know so little and seem to still accept that we know nothing: we should be routinely and systematically tracking, recording and collating pregnant women’s health outcomes. But we aren’t.”
We know embarrassingly little about anything that exclusively affects women:
We know extremely little about women’s reproductive system, endometriosis, menopause (despite the fact that 100% of women go through it), PMS, (…).
Now,
What is being done about this?
We have established that the lack of data on women’s bodies affects our ability to give women sound medical advice. So, are we fixing this?
Government-funded research (minority)
In 1993 the US passed the National Institute of Health Revitalization Act and since then it has been illegal not to include women in federally funded clinical trials. While this is a step in the right direction, issues remain: 1) the vast majority of clinical trials are privately funded (hence the act doesn’t apply), 2) it is questioned whether it is being practised/enforced (in the federally funded trial), 3) it does not require data to be analysed based on sex.
The EU has similar rules but went one step further, requiring both sexes to be studied in preclinical animal studies (since 2016).
The UK is “trailing behind everyone” – Anita Holdcroft, professor at Imperial College London, has written that for cardiovascular treatment “it is pertinent to use studies from North America and Europe where these issues have been investigated”.
Privately funded research (vast majority)
In short: “Independent drug manufacturers can do whatever they want.”
I looked at currently run research studies to get an idea of who is being recruited today and the results are not surprising: For example, Hammersmith Medicine Research is researching a potential new medicine to treat COVID-19 and “women must be postmenopausal for at least 1 year or surgically sterilised”. Some studies required that women of childbearing age “must have an IUD, IUS or ‘coil’”. Other studies e.g., on autism spectrum disorder (ASD) did not include women at all.
I will leave you with the following quote from Perez:
“Researchers continue to research men and act as if their findings apply to women. That this is still going on in the twenty-first century is a scandal. Women are dying, and the medical world is complicit.”
My Thoughts:
I have been aware of the shortcomings in research & medicine since my days in university. It astonishes me that 1) the grievances are not publicly discussed/common knowledge, and 2) that the progress of making things better is so incredibly slow.
I have a very low tolerance for injustice so needless to say that this topic makes me very angry. The following has helped me to deal with it: 1) raising awareness, 2) staying as healthy as I can (through lifestyle) to minimize chances of relying on medication/ the medical system*, 3) running my own little ‘research studies’ to find out what works for me and my body (especially when it comes to diet and exercise). Also, I deeply trust my intuition (‘the body’s wisdom’), 4) raising funds; I contacted Caroline Perez to find out if there is an organisation she trusts/recommends that funds medical research on women. (I will share details if she comes back. Also, let me know if you know one!)
I truly recommend her book (Invisible Women) as Perez covers data biases in the major areas of life (e.g., the workplace and public life). My article only scratches on one chapter (out of twenty) and doesn’t nearly cover enough information which (I believe) every person should be aware of.
(*To note, I am grateful for the general progress in medicine. Also, I acknowledge that not everything can be controlled by/through lifestyle choices.)
Lastly,
Question(s) for you:
- Were you aware of the shortcomings in scientific research/medicine?
- If you are a woman: Have you experienced (sex-dependent) issues with the medical system? (Of course, only share this with me if you are comfortable doing so. Also, the responses stay with me, I do not share them.)
- Not a question, just a Thank you for reading till the end. 🙂
Have a great day!
Best regards,
Sarah
Resources:
- Perez, C. C. (2019). Invisible Women. [United States], Abrams.
- Galvão-Moreira, L. V., de Andrade, C. M., de Oliveira, J. F. F., Bomfim, M. R. Q., Figueiredo, P. M. S., & Branco-de-Almeida, L. S. (2018). Sex Differences in Salivary Parameters of Caries Susceptibility in Healthy Individuals. Oral health & preventive dentistry, 16(1), 71–77. https://doi.org/10.3290/j.ohpd.a39684
- Marts, Sherry A. and Keitt, Sarah (2004), Principles of Sex-based Differences in Physiology: Foreword: a historical overview of advocacy for research in sex based biology’, Advances in Molecular and Cell Biology, 34, 1-333
- http://www.marieclaire.com/health-fitness/a26741/doctors-treat-women. like-men/; https://www.health.harvard.edu/heart-health/gender-matters-heart disease-risk-in-women
- Karp, Natasha A. et al (2017), ‘Prevalence of sexual dimorphism in mammalian phenotypic traits’, Nature Communications, 8:15475
- https://www.londontrials.com/trials
- Martha L. Blair (2007), ‘Sex-based differences in physiology: what should we teach in the medical curriculum?, Advanced Physiological Education, 31, 23-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4800017/ Jan 2016
- https://www.washingtonpost.com/national/health-science/why-do-autoimmune-diseases-affect-women-more-often-than-men
- http://docs.autismresearchcentre.com/papers/2010_Schwartz_SexSpecific_MolAut.pdf
- Clayton, Janine Austin (2015), Studying both sexes: a guiding principle for biomedicine’, http://www.fasebj.org/content/early/2015/10/28/f.15-279554.full.pdf+html
- https://theconversation.com/not-just-about-sex-throughout-our-bodies-thousands-of-genes-act-differently-in-men-and-women-86613
- http://www.wpro.who.int/topics/gender_issues/Takingsexandgenderinto-account.pdf
- Holderoft, Anita (2007) ‘Gender bias in research: how does it affect evidence based medicine?’, Journal of the Royal Society of Medicine, 100
- Ibarra, Manuel, Vázquez, Marta and Fagiolino, Pietro (2017), ‘Sex Effect on Average Bioequivalence’, Clinical Therapeutics, 39:1, 23-33
- Mergaert, Lut and Lombardo, Emanuela (2014), Resistance to implementing gender mainstreaming in EU research policy’, in Weiner, Elaine and Mace, Heather (eds), “The persistent invisibility of gender in EU policy; European Integration online Papers (EloP), special issue 1, Vol. 18, Article 5, 1-21
- Bruinvels, G. et al. (2016), Sport, exercise and the menstrual cycle: where is the research?’, British Journal of Sports Medicine, 51:6, 487-488
- Zopf, Y. et al. (2008), ‘Women encounter ADRs more often than do men, European Journal of Clinical Pharmacology, 64:999
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC198535/
- Soldin, Offie P., Chung, Sarah H. and Mattison, Donald R. (2011), ‘Sex Differences in Drug Disposition’, Journal of Biomedicine and Biotechnol-ogy, 2011:187103; Anderson, Gail D. (2005), ‘Sex And Racial Differences In Pharmacological Response: Where Is The Evidence? Pharmacogenetics, Pharmacokinetics, and Pharmacodynamics’, Journal of Women’s Health, 14:1, http://online.liebertpub.com.libproxy.ucl.ac.uk/doi/pdf/10.1089/jwh.2005.14.19
- Anderson (2005)
- Hughes (2007)
- Yoon, Dustin Y. et al. (2014), ‘Sex bias exists in basic science and translational surgical research’, Surgery, 156:3, 508-16 64 https://thinkprogress.org/scientists-avoid-studying-womens-bodies-because-they-get-periods-3fe9d6c39268/
- Yoon et al. (2014)
- Karp (2017)
- Hughes (2007)
- Yoon et al. (2014)
- Ortona, Elena, Delunardo, Federica, Baggio, Giovannella and Malorni, Walter (2016), ‘A sex and gender perspective in medicine: A new Mandatory Challenge For Human Health’, Ann Ist Super Sanita, 52:2, 146-8
- Woodruff, Teresa K. (2014), ‘Sex, equity, and science’, PNAS, 111:14, 5,063-4
- Nowak, Bernd et al. (2010), ‘Do gender differences exist in pacemaker implantation?-results of an obligatory external quality control program?,Europace, 12, 210-15
- http://www.smithsonianmag.com/innovation/the-worlds-first-true-artifcial-heart-now-beats-inside-a-75-year-old-patient-180948280/?no-ist
- http://www.syncardia.com/medical-professionals/two-sizes-70cc-50cc.html
- Sardeli, Amanda Veiga and Chacon-Mikahil, Mara Patricia T. (2016), ’Exercise-Induced Increase as a Risk Factor for Central Arterial Stiffness’, Journal of Archives in Military Medicine; http://circ.ahajournals.org/con-tent/110/18/2858; http://www.medscape.com/viewarticle/728571; https:/ www.ncbi.nlm.nih.gov/pubmed/22267567
- Collier, Scott R. (2008), ‘Sex Differences in the Effects of Aerobic and Anaerobic Exercise on Blood Pressure and Arterial Stiffness’, Gender Med-icine, 5:2
- Devries (2016)
- Tarnopolsky, M. A. (2008), ‘Sex Differences in Exercise Metabolism and the Role of 17-Beta Estradiol, Medicine and Science in Sports and Exercise, 40:4. 648-54
- Gender and Health Knowledse Agenda, May 2015 ZonMa, Nathedand,
- Yoon et al. (2014)
- Gender and Healch Knowledge Agenda, May 2015 (ZonMw, Netherlands)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC198535/135 https://www.hindawi.com/journals/bmri/2011/18710
- Anderson (2005)


